Nutrition
Food isn’t just “fuel” — it’s information for your brain, hormones, gut, immune system, and energy regulation.
If you’re dealing with low mood, stress, stubborn weight changes, blood sugar swings, digestive discomfort, pain / inflammation, perimenopause / menopause symptoms, or fatigue, nutrition support can be a practical (and empowering) place to start.
We offer evidence-informed nutrition coaching on its own or combined with complementary therapies (aromatherapy, auricular acupuncture, hypnotherapy or CBT coaching) to help you build changes that actually stick — without perfectionism or shame.


Why Support Matters
1) Mood, motivation, and resilience
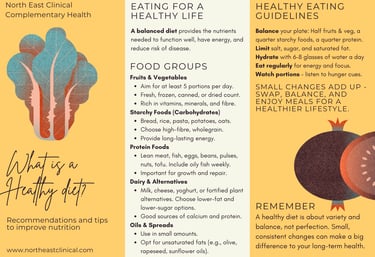
Diet quality is consistently linked with mental health outcomes, including depression risk, and dietary improvement has shown benefit as an adjunct approach for some people experiencing depression. What this means in practice: small, repeatable shifts (regular meals, protein and fibre at breakfast, omega-3-rich foods, colourful plants, fewer ultra-processed “quick hits”) can support steadier energy and a more stable emotional baseline.
2) Weight, appetite regulation, and long-term health
Weight change is rarely “just willpower.” Appetite signals, sleep, stress hormones, routine, medication effects, pain, and metabolic health all play a role. NICE guidance emphasises interventions that address diet + physical activity + behaviour change — because sustainable change is behavioural as much as nutritional.
3) Behaviour change is the missing link
Knowing what to do is one thing — doing it under real-life pressure is another. Evidence supports structured behaviour-change approaches (including CBT-informed methods and motivational interviewing-style coaching) to improve weight-loss outcomes and support maintenance.
Free & Simple Tools for Better Nutrition
Our Therapeutic Approach
Nutrition & Aroma-Acupuncture (stress & appetite support)
Best for: stress-eating, anxiety-driven snacking, low motivation, disrupted sleep, cravings, and “wired-and-tired” nervous system patterns.
Why combine?
When stress is high, the body often nudges you toward quick energy and comfort-seeking habits. Pairing nutrition coaching with a calming, body-based approach can make change feel less like a fight.
What the combined approach looks like
Nutrition plan that prioritises satiety and stability (protein + fibre + timing)
Aroma support to reinforce routines (e.g., an evening wind-down anchor, pre-meal pause, or “reset” moment)
Auricular acupuncture/auricular stimulation as a support for appetite /craving regulation and stress support.
Outcome focus: reduced stress-driven eating loops, improved sleep routine support, and more consistency with nourishing choices.


1:1 Nutrition Coaching (evidence-informed, realistic, supportive)
Best for: low mood (especially in winter), energy dips, perimenopause support, digestive discomfort patterns, inflammation/pain support, weight management, and “I know what to do but can’t stay consistent.”
What you can expect
A detailed intake: symptoms, health history, meds/supplements, routine, stress, sleep, preferences, cooking confidence, budget
A tailored plan built around your life (not a rigid diet)
Simple targets: meal structure, protein/fibre goals, hydration, blood sugar steadiness, and “minimum effective” weekly habits
Review and refine: we track what works, troubleshoot what doesn’t, and keep it achievable
Outcome focus: steadier energy, fewer crashes, more predictable appetite, improved confidence with food choices, and a plan you can maintain.
Best for: emotional eating, binge-restrict cycles, all-or-nothing thinking, confidence issues around food, and long-standing behaviour patterns.
Why this works (when appropriate):
CBT-informed approaches support weight loss and maintenance by targeting the thoughts, emotions, and cues that drive eating behaviours — not just the food itself.
Hypnotherapy can be helpful where stress responses, automatic habits, or gut–brain patterns are central. For example, gut-directed hypnotherapy shows benefit for IBS symptoms in research (useful when digestive symptoms and anxiety are intertwined).
What you can expect
Identify triggers (such as stress, fatigue, social situations, sensory cravings, and reward patterns)
Build replacement responses (such as urge surfing, “if–then” plans, and compassionate self-talk)
Hypnotherapy sessions to reinforce calm, confidence, and identity-based change (“I’m someone who looks after myself consistently”)
Clear nutrition structure so your brain isn’t trying to make food decisions under stress
Outcome focus: fewer “auto-pilot” choices, more self-trust, calmer relationship with food, and sustainable routines.
Nutrition & Hypnotherapy or CBT (for habits that won’t shift)





Important note: If we suspect an eating disorder or you’re experiencing red flags (e.g., rapid unintended weight loss, persistent GI bleeding, severe restriction, purging, fainting, or significant mental health risk), we’ll recommend GP-led assessment and/or specialist care in line with NICE guidance.
Our Client Experience
Winter mood & energy crashes
Starting point (info gathering):
A 42-year-old with low winter mood, afternoon fatigue, carb cravings, and poor sleep. Intake shows irregular meals, low protein at breakfast, long gaps between meals, and high reliance on quick snacks during stressful workdays.
Plan:
Week 1–2: Stabilise mornings (protein + fibre breakfast), add a planned lunch, and a mid-afternoon “bridge snack”
Week 3–6: Build a simple “comforting but balanced” dinner rotation; introduce omega-3-rich foods and colourful plants
Add-on: Aroma anchor for evening wind-down + “pause cue” before snacking
Outcome:
By week 6–8, the client reports fewer energy crashes, improved sleep routine consistency, fewer cravings, and more stable mood. The focus stays on repeatable habits, not perfect eating — and we keep adjusting based on real life.
Stress-eating & stubborn weight changes
Starting point (info gathering):
A 55-year-old in perimenopause/menopause transition with stress-eating, poor appetite regulation in the evenings, and a long history of dieting. Intake highlights all-or-nothing thinking (“I’ve blown it, so I may as well…”), high stress load, and inconsistent meal structure.
Plan:
Nutrition: regular meals, protein targets, high-fibre “volume” foods, and a realistic approach to treats
CBT-style coaching: identify trigger chain (stress → fatigue → snack → guilt → restrict → rebound) and build an “interrupt plan”
Hypnotherapy: reinforce calmer nervous system responses, reduce automatic evening snacking cues, build self-efficacy
Optional auricular acupuncture as an adjunct for cravings/appetite regulation
Outcome:
By week 10–12, the client reports fewer binge-restrict cycles, improved consistency, less guilt, and clearer hunger/fullness cues. Weight and measurements may change gradually, but the key win is sustainable behaviour change and a calmer relationship with food — the foundation NICE-aligned approaches prioritise.


References
Adler, E. C., et al. (2025). Gut-directed hypnotherapy for irritable bowel syndrome: A systematic review and meta-analysis. Neurogastroenterology & Motility.
Bahri, A. A., et al. (2025). Motivational interviewing to promote healthy lifestyle behaviors. [Review article in PubMed Central].
Berry, S. K., et al. (2023). Digital gut-directed hypnotherapy for irritable bowel syndrome: A randomized parallel-group study. Clinical Gastroenterology and Hepatology.
Chen, L., et al. (2022). The efficacy and safety of auriculotherapy for weight loss: A systematic review. Integrative Medicine Research.
Compañ-Gabucio, L. M., et al. (2023). Cognitive behavioural therapies for weight-loss in adults. [Review article in PubMed Central].
Hua, K., et al. (2024). Effects of auricular stimulation on weight- and obesity-related outcomes. [Article in PubMed Central].
Jacka, F. N., O’Neil, A., Opie, R., et al. (2017). A randomised controlled trial of dietary improvement for adults with major depression (the “SMILES” trial). BMC Medicine, 15, 23. https://doi.org/10.1186/s12916-017-0791-y
Kurnik Mesarič, K., et al. (2023). Cognitive behavioral therapy for lifestyle changes in obesity: A meta-analysis. Scientific Reports.
Molero, P., et al. (2025). Diet quality and depression: A systematic review and meta-analysis of prospective studies. Journal of Affective Disorders.
National Institute for Health and Care Excellence. (2017). Eating disorders: Recognition and treatment (NG69).
National Institute for Health and Care Excellence. (2025). Overweight and obesity management (NG246).
Paris, T., et al. (2024). Dietary interventions and depression outcomes in adults with metabolic conditions: A systematic review and meta-analysis of randomized trials. [Article in PubMed Central].
Zhu, S. F., et al. (2024). Effectiveness of behavioural interventions with motivational interviewing: Systematic review and meta-analysis. The BMJ.
THANK YOU FOR VISITING
Please like and follow our socials, or sign up to our seasonal newsletter.
Contact us
hello@northeastclinical.co.uk
WhatsApp Chat 07368 638324
© North East Clinical 2025. All rights reserved.